Introduction
Some mushrooms may be nutritious foods [
1], and it has been estimated that 1.5 million different species of them exist worldwide [
2]. However, due to the existence of poisonous mushrooms, it’s crucial to identify the type before consumption [
1]. Poisonous mushrooms contain toxic substances, such as amatoxins, muscarine, coprine, orellanus, and psilocybin, that are hazardous to human health [
3,
4]. They are subdivided into groups based on the clinical signs and symptoms they cause in humans at presentation. Common syndromes associated with mushroom poisoning include damage to major internal organs, neurotoxicity, metabolic, endocrine and gastrointestinal disorders [
5]. Most poisoning cases present with gastroenteritis and psycho-neurological disorders; however, the patients usually recover without serious clinical consequences [
6]. The most dangerous fungal species known today are Amanita mushrooms (Amanita phalloides, Amanita virosa, and Amanita verna), which cause severe clinical symptoms or even fatal outcome [
7].
Three stages have been described for Amanita poisoning: a) gastrointestinal symptoms in the first 6 to 24 hours, b) hepatic sign and symptoms appear with a 12-48 hour latency, and c) acute kidney and liver failure develop 24-72 hours later [
8]. Although certain methods have been suggested to identify toxic mushrooms, there is no definitive standadrds for their identification [
4]. Features such as the mushroom’s shape, surface, and color of the cap, gill, stalk, and the odor might help diffrentiate safe mushrooms from the poisonous ones [
9]. The prevalence of mushroom toxicity has been estimated at 7428 cases per year in the United States [
10]. In Iran, a total of 50 species of poisonous mushrooms have been identified. In the spring, sporadic cases of mushroom poisoning occur in Iran [
11]. In a study at a poisoning center in Tehran, 37 cases of mushroom poisoning were reported over a 10-year period [
12].
In the diagnostic process, the clinical differences for various poisoning syndromes should be distinguished [
5]. Identification of the consumed mushrooms and the time elapsed between the consumption and onset of symptoms are the key to the diagnosis. Macroscopic identification of the ingested mushrooms or the leftovers, and the microscopic features of the spores in the plant are the most useful data for the diagnosis [
8]. To date, such a study has not been conducted.
Aim of the study: Khorramabad city is located in Lorestan province, a mountainous area in western Iran. Due to its unique geographical nature, a high variety of herbal plants is grown in this area, thus leading to a high incidence poisoning [
13]. In 2018, the second highest mushroom poisoning outbreak in Iran occurred in Lorestan province [
11]. Given the high rate of mushroom poisoning reported in Lorestan Province, this study aimed to evaluate the frequency of clinical and paraclinical manifestations of poisoning cases due to the consumption of mushrooms, as referred to Shahid Rahimi Hospital in Khorramabad, Iran, during a one year period (2018-2019).
Materials and Methods
Study design and participants: This cross-sectional, descriptive study was undertaken to investigate the frequency of clinical and paraclinical manifestations due to mushroom poisoning at Shahid Rahimi Hospital in Khorramabad, Iran. The study subjects were patients who were reffered to, diagnosed and hospitalized due to mushroom poisoning. Patients with incomplete medical records and those who did not consent to participate in the study were excluded.
Data collection: The frequency of clinical manifestations of mushroom poisoning, such as gastrointestinal or neurological symptoms, and others, such as the age, sex, seasons, type of mushrooms consumed, patient’s residence, latent phase, clinical and laboratory findings, length of hospital stay, therapeutic interventions, and the underlying diseases were reviewed and recorded. Initially, the responsible factors were tabulated as a checklist of full description and review of the each useful study found over a literature search.
Data analyses: After collecting the relevant data and clinical information, descriptive statistical methods were used to analyze the data. A statistical software (SPSS software, version 18) was utilized to analyze the data. Using descriptive methods, the frequency, percentage, Mean±SD, and other findings are presented in this article as one Figure and nine Tables.
Ethical considerations: The study protocol was approved by the Research Ethics Committee at Lorestan University of Medical Sciences (Code #: IR.LUMS.REC.1399.064). The data for each patient were collected from the available clinical records, such that there was no direct communication with the patients. They had signed a consent form at admission into the hospital. All patients’ information were kept strictly confidential and no disclosure was made to any sources other than the attending physicians. In order to avaoid registering the patients by their names, we used a specific code to refer to each individual. The information was kept confidential and recorded in numerical codes, using SPSS software, version 18. Prior to conducting this study, necessary arrangements were made with the administration of the Lorestan University of Medical Sciences’ Hospital via submitting a formal document, containing the study protocol and the aims. Subsequently, the Ethics Committee reviewed the study protocol and approved it.
Results
In this study, 124 patients with mushroom poisoning participated, 73 of whom (58.9%) were male and 51 (41.1%) were female. The patients’ mean age was 36.65±19.7 years old, with the minimum being 2 and the maximum 83 years old.
Figure 1 represents the study population age distribution.
The mean duration of hospital stay was 2.19±1.7 days, ranging from zero to seven days. In terms of patients’ occupation, the highest frequency of the study population were housewives (36.3%). Most of the poisoning cases occurred in the Spring (91.1%), and the most frequently used medications to treat the symptoms and side effects were Livergol (48.4%), and Atropin (33.1%) (
Table 1).

The Mean±SD for the duration of the mushroom consumption until being symptomatic was 4.58 hours, ranging from zero to 24 hours. The duration from the mushroom consumption to the patients being referred to the hospital was 6.05 hours (minimum, 0.5, maximum 24 hours).
Table 2 lists the data for the Mean±SD, minimum and maximum laboratory findings.

Most of the subjects had collected the mushrooms from the nature (79.8%). As seen in
Table 3, the most common clinical symptoms reported by the patients were nausea and vomiting (81.5%), sweating (41.1%), and abdominal pain (37.1%).

Of the total cases, 23 of them (18.5%) were examined by a second physician before being admitted to the hospital. The most frequent underlying diseases were as follows: hypertension (8.9%); coronary artery disease (6.5%); diabetes (5.6%); renal disease (1.6%); hematological disease (1.6%); and liver disease (0.8%). Considering the final outcomes, 75 patients (60.5%) were hospitalized, while 36 of them (29%) left the hospital voluntarily, 9(7.3%) were admitted to the ICU, 2(1.6%) were discharged from emergency room, 1(0.8%) was referred to a specialized center, and one patient (0.8%) died.
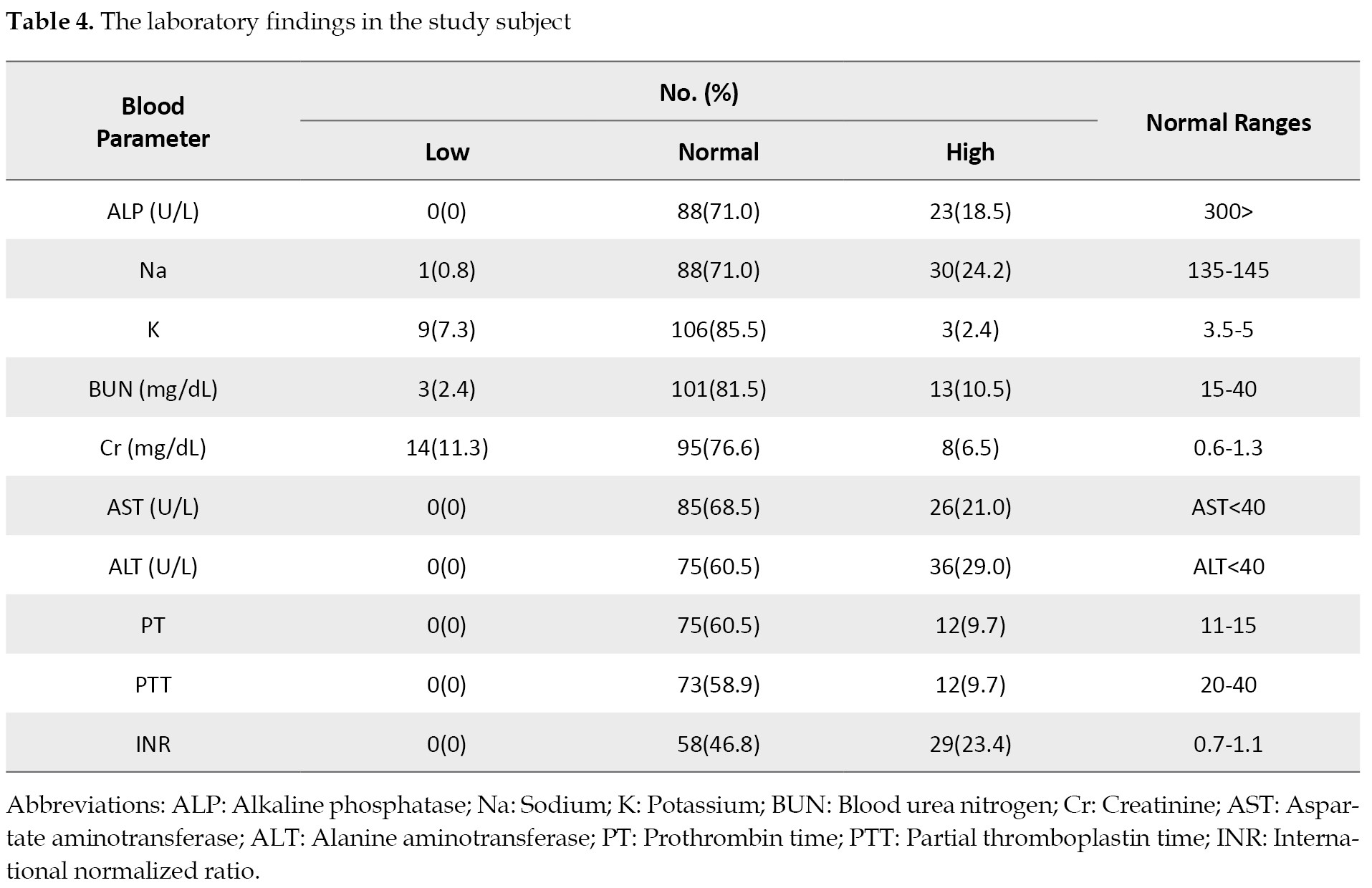
Table 4 presents the distribution of the laboratory findings for the subjects.
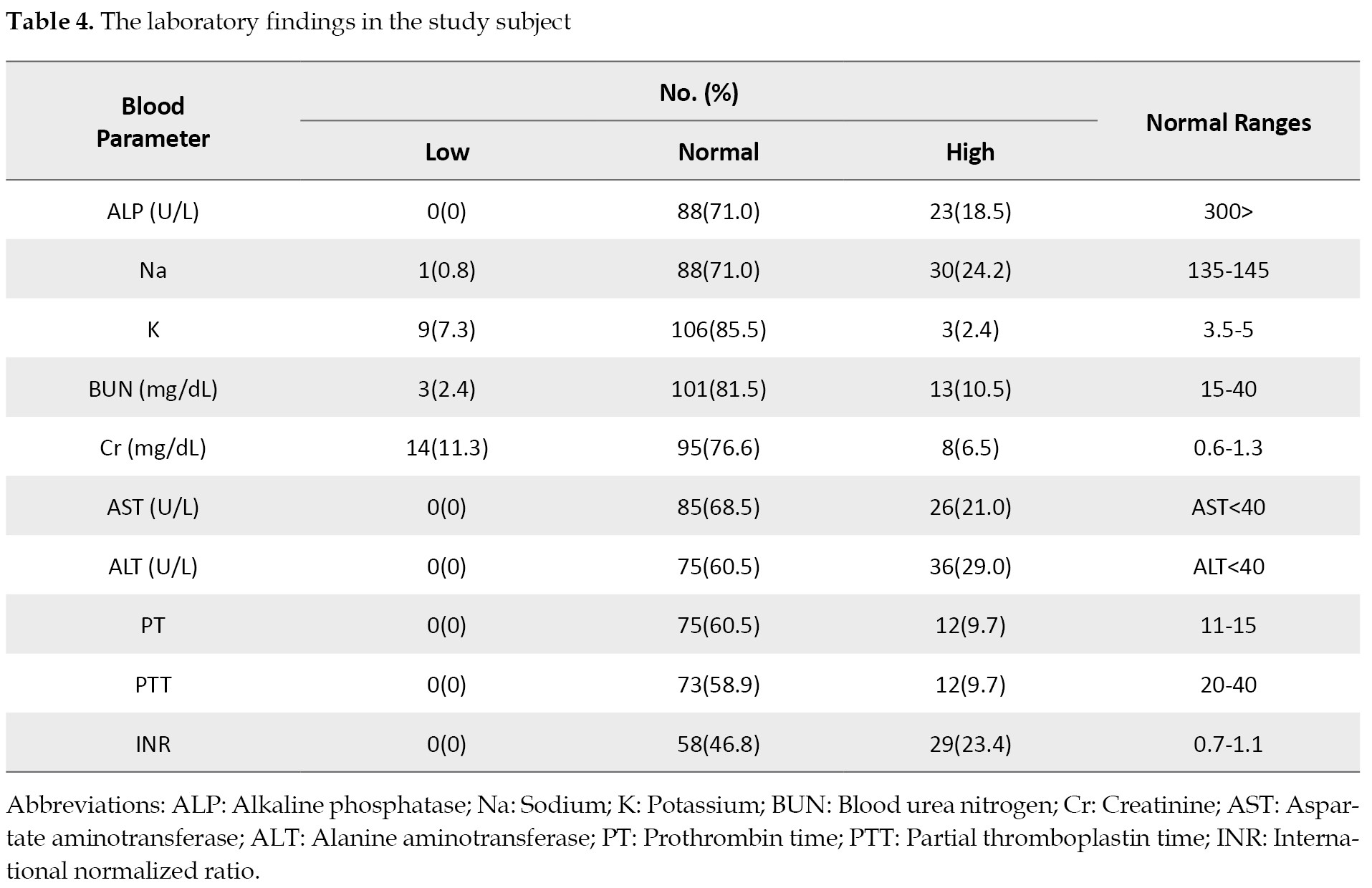 Table 5
Table 5 provides information on the distribution of the subjects’ clinical signs based on gender.
 Table 6
Table 6 lists the data on the distribution of clinical signs based on the patients’ occupation.
 Table 7
Table 7 presents information on the clinical signs for each patient based on the season.
 Table 8
Table 8 shows the information on the clinical signs based on the patients’ underlying diseases.

Finally,
Table 9 presents the patients’ signs based on the clinical outcomes.
 Discussion
Discussion
This study evaluated the clinical and paraclinical manifestations observed in patients with mushroom poisoning in Khorramabad, Lorestan province, Iran. In Iran, a total number of 50 species of poisonous mushrooms have been identified and Amanita is the most dangerous species identified in the country [
14]. In the 2018 mushroom poisoning outbreak in Iran, the following species were involved: Lepiota brunneioncarnata, Hypholoma fascicalare, and Coprinopsis atramentaria [
11]. In a previous study in Lorestan province, muscarin toxin was reported as the most common cause of mushroom poisoning [
13].
Demographic characteristics: Regarding the demographic characteristics of patients, most of our subjects were male. Consistent with our findings, Chen et al. [
15] and Pajoumand et al [
12] also observed a higher incidence of poisoning in men. The mean age of our patients was 36.65, consistent with 35 year old as reported by Erenler et al. [
16]. The mean length of hospital stay in our study was 2.19 days. However, in another study by Keller et al. [
17], 78.4% of cases stayed in the ER for less than 24 hours, similar to 1.89 days that was observed by Khatir et al. [
18].
Our findings showed that 79.8% of the cases had consumed self-picked poisonous mushrooms, which is similar to 83% of the patients, that was found by Jiang et al. [
19]. Further, we found the mean time elapsed between the mushroom consumption and the onset of symptoms was 4.58 hours. Also, the interval between the mushroom consumption and the admission to the hospital was 6.05 hours. Our findings were similar to those reported by two earlier studies [
17,
19] who observed that in 68.6% and 62% of the subjects, respectively, the clinical symptoms began within the first 6 hours of the mushroom ingestion. Also, with respect to the season of the year when the poisoning happened, we found that 91.1% of them occurred in the Spring. Similarly, Varshouchi et al. reported that 68% of poisoning cases occurred in the Spring [
20]. However, Gold et al. [
21] have reported that a greater number of similar poisoning (36.8%) happened in the Summer while only 22.5% of them occurred in the Spring.
Clinical and paraclinical findings: In our study, the most frequently reported clinical symptoms by the patients were nausea and vomiting, followed by sweating, abdominal pain, and diarrhea. Nausea and vomiting was the most common symptom in both male and female, and in patients with various underlying diseases. However, in retired patients and employees, and in those who were admitted in the Fall, sweating and abdominal pain were the most frequently reported symptoms. Similarly in 2016, Chan et al. reported 67 mushroom poisoning cases in Hong Kong, 90% of whom presented with gastrointestinal symptoms [
22]. In these patients, all of the laboratory tests were within normal ranges. Evidently, the identification of the type of mushrooms consumed and the knowledge of clinical variations among poisoning syndromes remain the major diagnostic challenge to date [
5,
8]. However, a significantly higher neutrophil-to-lymphocyte ratio and lower platelet count have been observed in patients with mushroom poisoning [
23]. In our study population, impaired liver function test was the most common paraclinical finding. Similar observations have also been reported in two previous studies performed in Iran [
14,
24].
Therapeutic interventions: Currently, there is no definitive and preferred treatment for the human cases with mushroom poisoning. Although there are controversies over the use of activated charcoal, this approach has been recommended by many earlier studies. Supportive treatments, such as correction of electrolyte abnormalities and dehydration should also be considered [
25]. Ordinarily, drugs and antidotes are used in some poisoning cases. In case of a neurological sign, such as seizure, benzodiazepines and pyridoxine may be prescribed. Also, atropine is beneficial to counter the cholinergic presentations. In cases of Amanita toxicity, patients may benefit from Silibinin, N-acetylcysteine, or even liver transplant if a fulminant hepatic failure has occurred [
17].
In our study, the most common therapeutic interventions were Livergol (containing Silybum marianum), atropine, and N-acetylcysteine. In Keller et al.’s study, 56.9% of the cases received activated charcoal, and the other 24% were treated with N-acetylcysteine [
17]. The overall mortality rate of mushroom poisoning cases is fairly low at 2.17% [
6], although, a wide range of mortality has been reported in the reviewed literature. In our study, this rate was very low, at 0.8% of the mushroom poisoning cases. Chen et al. reported only two deaths among the 429 patients they treated with mushroom poisoning in China [
15]. Conversely, De Olano et al. have reported a higher rate of mortality at 8.8% among their poisoning cases that ingested cyclopeptide mushrooms in the United States [
26].
Conclusions
In this study, a large majority of the patients developed gastrointestinal (GI) symptoms, such as nausea and vomiting, whom were managed clinically with medications; however, there was one fatal case. In addition to the GI symptoms, our subjects complained of sweating and abdominal pain. Among them, the most frequent underlying diseases were hypertension, coronary artery disease, diabetes, and renal, hematological or liver diseases. Health authorities are highly advised to educate the public on poisoning due to mushroom ingestion. Such efforts will positively lead to reductions the number of poisoning cases, especially in the spring and summer. It will also shorten the patients’ hospital stay, and ultimately reduce the subsequent mortality.
Limitations of the study: We had the following limitations in this study: a) the medical records of some patients were incomplete, which led to their exclusion from the study; b) the types of consumed mushrooms had not been recorded in all patients record.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee at Lorestan University of Medical Sciences (Code: IR.LUMS.REC.1399.064).
Funding
This study did not receive funds from any entity other than the authors.
Authors' contributions
Conceptualization, supervision, methodology and funding acquisition and resources: Ghafarali Mahmoudi; Investigation, writing-original draft, and writing-review & editing: All authors; Data collection: Mohammad Hojat Bazrafkan; Data analysis: Soudabeh Zare.
Conflict of interest
The authors declare no conflict of interest with any entities to disclose.
Acknowledgements
The authors gratefully appreciate the participation of the patients in this cross-sectional clinical trial. The authors are also thankful to the administration and staff of Shahid Rahimi Hospital in Khorramabad, Iran, for their generous cooperation with this research project.
References
- Zahan N, Hasan Z, Malek A, Reya SS. A deep learning-based approach for edible, inedible and poisonous mushroom classification. Pape rpresented at: 2021 International Conference on Information and Communication Technology for Sustainable Development (ICICT4SD). 27-28 February 2021; Dhaka, Bangladesh. [DOI:10.1109/ICICT4SD50815.2021.9396845]
- Chitayae N, Sunyoto A. Performance comparison of mushroom types classification using K-nearest neighbor method and decision tree method. Paper presented at: 2020 3rd International Conference on Information and Communications Technology (ICOIACT). 24-25 November 2020; Yogyakarta, Indonesia. [DOI:10.1109/ICOIACT50329.2020.9332148]
- Sevindik M. Poisonous mushroom (nonedible) as an antioxidant source. In: Ekiert HM, Ramawat KG, Arora J, editors. Plant antioxidants and health. Reference series in phytochemistry. Cham: Springer; 2020.[DOI:10.1007/978-3-030-45299-5_8-1]
- Jo WS, Hossain MA, Park SC. Toxicological profiles of poisonous, edible, and medicinal mushrooms. Mycobiology. 2014; 42(3):215-20. [PMID] [PMCID]
- White J, Weinstein SA, De Haro L, Bédry R, Schaper A, Rumack BH, et al. Mushroom poisoning: A proposed new clinical classification. Toxicon. 2019; 157:53-65. [DOI:10.1016/j.toxicon.2018.11.007] [PMID]
- Li H, Zhang H, Zhang Y, Zhou J, Yin Y, He Q, et al. Mushroom poisoning outbreaks─ China, 2021. China CDC Weekly. 2022; 4(3):35-40. [PMID]
- Tavassoli M, Afshari A, Arsene AL, Mégarbane B, Dumanov J, Paoliello MMB, et al. Toxicological profile of Amanita virosa - A narrative review. Toxicology Reports. 2019; 6:143-50. [DOI:10.1016/j.toxrep.2019.01.002] [PMID] [PMCID]
- Wennig R, Eyer F, Schaper A, Zilker T, Andresen-Streichert H. Mushroom poisoning. Deutsches Arzteblatt International. 2020; 117(42):701-8. [DOI:10.3238/arztebl.2020.0701] [PMID] [PMCID]
- Ismail S, Zainal AR, Mustapha A. Behavioural features for mushroom classification. Paper presented at: 2018 IEEE Symposium on Computer Applications & Industrial Electronics (ISCAIE). 28-29 April 2018; Penang, Malaysia. [DOI:10.1109/ISCAIE.2018.8405508]
- Brandenburg WE, Ward KJ. Mushroom poisoning epidemiology in the United States. Mycologia. 2018; 110(4):637-41. [PMID]
- Soltaninejad K. Outbreak of mushroom poisoning in Iran: April-May, 2018. The International Journal of Occupational and Environmental Medicine. 2018; 9(3):152-6. [PMID] [PMCID]
- Pajoumand A, Shadnia S, Efricheh H, Mandegary A, Hassanian-Moghadam H, Abdollahi M. A retrospective study of mushroom poisoning in Iran. Human & Experimental Toxicology. 2005; 24(12):609-13. [DOI:10.1191/0960327105ht572oa] [PMID]
- Mahmoudi GA, Solhi H, Tarrahi MJ. The study of poisoning whit mushroom and toxic plants (tattore and ricinus communis) incidence in patients who admitted in Shohadaie Ashaier and Madani Hospitals in the Spring and Summer of 2007. Iranian Journal Toxicol. 2007; 1(3): 4-4. [Link]
- Dadpour B, Tajoddini S, Rajabi M, Afshari R. Mushroom poisoning in the Northeast of Iran; A retrospective 6-year epidemiologic study. Emergency (Tehran, Iran). 2017; 5(1):e23. [PMID]
- Chen L, Sun L, Zhang R, Liao N, Qi X, Chen J, et al, Epidemiological analysis of wild mushroom poisoning in Zhejiang province, China, 2016-2018. Food Science & Nutrition. 2022; 10(1):60-6. [DOI:10.1002/fsn3.2646] [PMID] [PMCID]
- Erenler AK, Doğan T, Koçak C, Ece Y. Investigation of toxic effects of mushroom poisoning on the cardiovascular system. Basic & Clinical Pharmacology & Toxicology. 2016; 119(3):317-21. [DOI:10.1111/bcpt.12569] [PMID]
- Keller SA, Klukowska-Rötzler J, Schenk-Jaeger KM, Kupferschmidt H, Exadaktylos AK, Lehmann B, et al. Mushroom poisoning-A 17 year retrospective study at a level I university emergency department in Switzerland. International Journal of Environmental Research and Public Health. 2018; 15(12):2855. [DOI:10.3390/ijerph15122855] [PMID] [PMCID]
- Khatir IG, Hosseininejad SM, Ghasempouri SK, Asadollahpoor A, Moradi S, Jahanian F. Demographic and epidemiologic evaluation of mushroompoisoning: A retrospective study in 4-year admissions of Razi Hospital (Qaemshahr, Mazandaran, Iran). Medicinski Glasnik : Official Publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina. 2020; 17(1):117-22. [PMID]
- Jiang L, Luo M, Hao L. Epidemiological characteristics of mushroom poisoning in Yunnan Province, China, 2004-2016. Southeast Asian Journal of Tropical Medicine and Public Health. 2018; 49(3):509-15. [Link]
- Varshouchi M, Naghili B. Mushroom poisoning in Northwest of Iran. Iranian Journal of Clinical Infectious Diseases. 2007; 2(4):177-80. [Link]
- Gold JAW, Kiernan E, Yeh M, Jackson BR, Benedict K. Health care utilization and outcomes associated with accidental poisonous mushroom ingestions - United States, 2016-2018. MMWR. Morbidity and Mortality Weekly Report. 70(10):337–41. [DOI:10.15585/mmwr.mm7010a1] [PMID] [PMCID]
- Chan CK, Lam HC, Chiu SW, Tse ML, Lau FL. Mushroom poisoning in Hong Kong: A ten-year review. Hong Kong Medical Journal. 2016; 22(2):124-30. [DOI:10.12809/hkmj154706] [PMID]
- Doğan M, Karahan I. Evaluation of complete blood count parameters, cell ratios, and cell volume indices in mushroom poisonings. Human & Experimental Toxicology. 2019; 38(10):1127-31. [DOI:10.1177/0960327119855131] [PMID]
- Badsar A, Rahbar TM, Amir MA, Rouhi RM, Chatrnour G, Khajeh JS. Mushroom poisoning in the Southwest Region of the Caspian Sea, Iran: A retrospective study. Iranian Journal of Toxicology. 2013; 7(20):798-803. [Link]
- Beaumier M, Rioult JP, Georges M, Brocheriou I, Lobbedez T, Lanot A. Mushroom poisoning presenting with acute kidney injury and elevated transaminases. Kidney International Reports. 2019; 4(6):877-81. [DOI:10.1016/j.ekir.2019.02.016] [PMID] [PMCID]
- De Olano J, Wang JJ, Villeneuve E, Gosselin S, Biary R, Su MK, et al. Current fatality rate of suspected cyclopeptide mushroom poisoning in the United States. Clinical Toxicology. 2021; 59(1):24-7. [DOI:10.1080/15563650.2020.1747624] [PMID]










































 , Mohammad Hojat Bazrafkan2
, Mohammad Hojat Bazrafkan2 

 , Golnaz Mahmoudvand2
, Golnaz Mahmoudvand2 

 , Peiman Astaraki1
, Peiman Astaraki1 

 , Soudabeh Zare3
, Soudabeh Zare3 

 , Arian Karimi Rouzbahani *
, Arian Karimi Rouzbahani * 

 4
4