Introduction
The trafficking of illicit substances considered an expanding and profitable means of commerce throughout the world. Body packers are individuals who illegally carry illicit substances, often cocaine and heroin, concealed within their bodies in packets made of a variety of materials [
1]. The packets can be ingested or inserted in the rectum or vagina before crossing borders between cities and counties without being detected [
1]. Body stuffers, sometimes called mini packers, are individuals who ingest illicit substances in loose packaging quickly to avoid detection, often in a situation of impending arrest [
2]. Differentiating between body packers and body stuffers originate from their purpose for concealment, quantity of drug ingested, and the manner of cover-up [
1].
Body packers have a tendency to hide large drug quantities of extreme purity in fixed firm, and wearable packages, whereas body stuffers typically swallow smaller quantity, less pure, and loosely packaged drugs quickly in an effort to avoid pending detection or arrest [
3,
4]. It should be noted that in both groups, each package usually contains a life-threatening amount of drug. Therefore, body stuffers are exposed to a remarkable danger of leaking significant quantity of drug due to the unprepared intake in unsafe packaging, which was never planned for gastrointestinal transit, with destructive results and reported fatalities [
4]. The common cause of death between body packers and stuffers is the rupture of the inserted packages, causing acute intoxication and consequences due to the size and number of packets ingested [
5,
6]. Swallowing several packets can lead to decreased gastrointestinal transit, GI obstructions, bowel perforation, and even death [
6]. In addition, the complications due to unexpected packet leakage may vary, because of substance variations, presenting diagnostic and therapeutic challenges for the emergency medicine physicians [
5]. Given the difficulty in taking a truthful history from the victims, and inadequate interpretation of the clinical presentations, laboratory tests and radiographic techniques play an important role in the diagnosis, follow-up, and management of these cases [
5].
In cases where internal concealment of drugs is suspected, their existence, number and location must be accurately determined. Leaky packages may lead to overdose, thus immediate and exact identification and location of the packet are essential. Reportedly, abdominal X- ray and CT images provide different capabilities in detecting body packets. The concealed substances are usually wrapped in condoms or similar materials and, in some cases, air can leak into these packets and create a characteristic ring or double shadow, clearly detectable by radiography. Abdominal X-ray images have the ability to detect over 80% of such concealed packages in human body [
1].
Computed Tomography (CT) is superior to plain abdominal X-ray images in detecting concealed packets and is currently considered the reference method. This is especially preferable in situations where abdominal X-ray images have been negative. The management approach depends on the quantity and quality of ingested packages in addition to the clinical presentations documented for the victims. Characteristically, asymptomatic patients need close observation, monitoring and tracing of package movement, whereas symptomatic patients necessitate urgent treatment, such as surgical intervention. Despite the high prevalence of body packing and stuffing, there are still controversies surrounding the management of these patients [
7]. Therefore, the aim of this study was to explore the characteristic presentations, clinical course, diagnostic and therapeutic measures and the subsequent clinical outcomes following either body packing or body stuffing.
Materials and Methods
Study design and setting: This cross-sectional retrospective study included all suspected body packer and body stuffer cases who had been admitted to Khorshid University Hospital affiliated with Isfahan University of Medical Sciences from Mar. 2013 to Feb. 2018. The Ethics Committee at Isfahan University of Medical Sciences approved the study protocol (Research project ID: 297069).
Participants: The 86 hospitalized patients that were included in this study were all body packers or body stuffers admitted to the toxicology ward or intensive care unit of the hospital (Mar. 2013-Feb. 2018). Body packers were defined as the admitted cases following confirmed concealment of illicit substances while crossing borders, based on self-confession or police reports. Body stuffers were classified as admitted cases to the hospital following confirmed ingestion of loosely packed, illicit substances to avoid arrest by the police. There were no limitations with respect to gender, age or criteria for the detected packages during the body search of the individuals.
Data collection: We used an author-designed questionnaire to collect the study data by a trained physician in every case. The questionnaire contained approximately 30 items about the patients’ demographics, such as: age, sex, history of substance abuse or dependence, criminal history, type of illicit substance and number of packets, time between ingestion and hospital admission, clinical presentations, level of consciousness, pupil size, heart and respiratory rates, mean blood pressure, blood gas levels on arrival and during hospitalization, need for intubation, duration of hospital stay, treatment modalities (conservative vs intervention), type of imaging, i.e., abdominal radiography vs CT, and the patients’ outcomes, i.e., full recovery versus death.
Statistical analyses: The data were analyzed using SPSS v. 20. The findings were presented as Mean±SD for continuous variables and frequency (%) for categorical variables, values of the difference between two data sets were considered as statistically significant at P≤0.05. Comparisons were also made, using Mann-Whitney U-test for the non-parametric variables and independent t-test was used for the parametric variables.
Results
Baseline characteristics: Eighty-six cases (68 body stuffers and 18 body packers) were included in this study. Seventy-eight patients (90.7%) were male and eight (9.3%) were female (P=0.834), most of whom were between the ages of 20 to 40 years.
Table 1 represents the demographic characteristics of the patients. Of the 86 patients, 62 (72%) had a positive history of substance dependence to heroin, opium or crystal methamphetamine.

The Mean±SD of their hospital stay was 1.71±0.46 days for body stuffers and 1.89±0.60 days for body packers. The median number of packets was two for body stuffers and six for body packers. The patients’ addiction, criminal and/or conviction histories, and the mean time elapsed between ingestion and hospital admission was 4.76 hours for body stuffers and 148.82 hours for body packers. The number of the most common concealed substances were as follows:
• Heroin: 40 cases of body stuffers (58.8%) and 12 cases of the body packers (66.7%).
• Methamphetamine: 16 cases of body stuffers (23.5%) and 6 cases of body packers (33.3%).
Clinical signs and symptoms: The patients’ clinical signs and symptoms are presented in
Table 2.

-_5_year.PNG)
The pupil size, heart and respiratory rates, venous blood gas values both at admission and during hospital stay were not statistically different between the two groups. The mean systolic and diastolic blood pressure at admission was higher among body stuffers, and the frequency of confusion was higher among the body packers (P=0.007), compared to the other group.
Imaging interventions: In this study, all cases underwent abdominal X-ray imaging. This test was positive for the detection of packets in 10 cases (14.7%) of the body stuffers and in 11 cases (61.1%) of the body packers. Although the number of packets in either group was estimated based on reliable evidence or patients’ confession, they were not exactly and physically counted. Also, CT scan was performed on 30 individuals (44%) among the body stuffers and on all 18 people (100%) of the body packers. The CT images enabled the identification of the packages and their numbers in 9 cases (30%) of the body stuffers and 17 cases (94.4%) of the body packers.
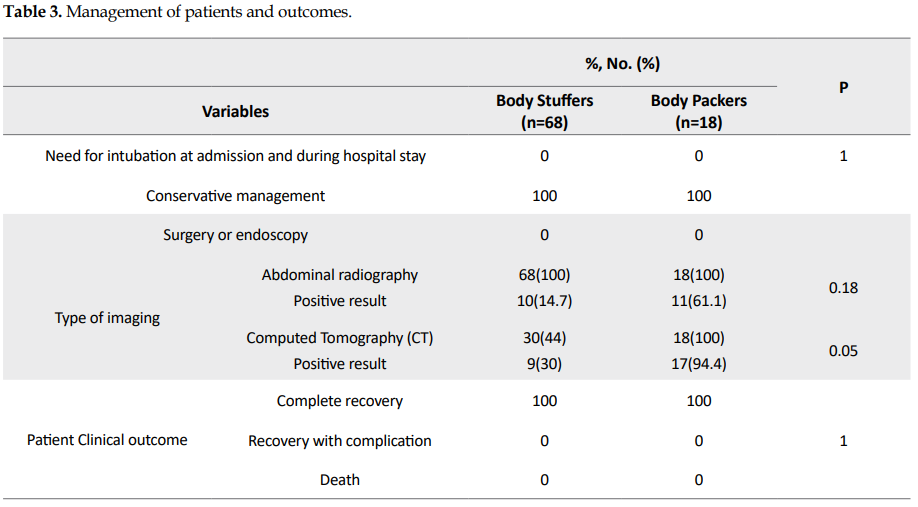
Clinical outcomes: The clinical management and outcomes of patients are shown in
Table 3.
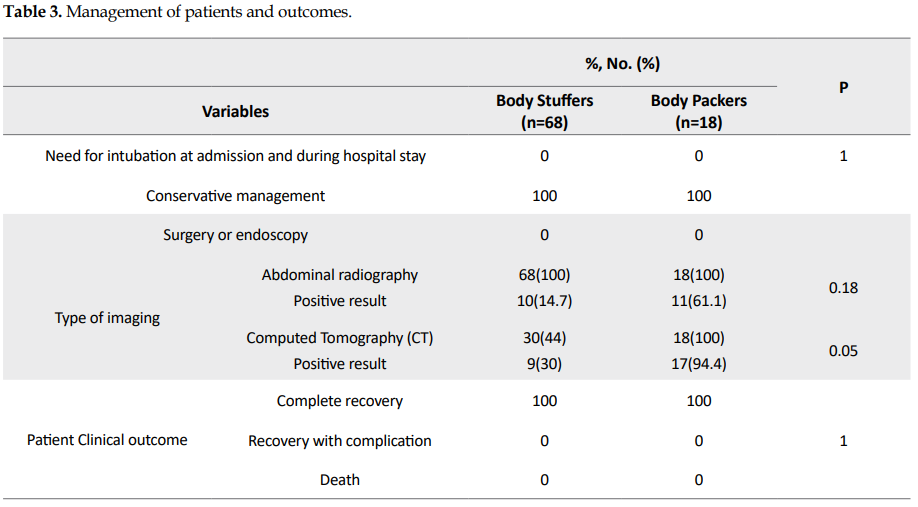
The need for intubation, and patients’ treatment outcomes were not statically different between the two groups. Invasive procedures, such as endoscopy and laparoscopy were not required to remove the packages from either group. All of the patients included in the study gained full recovery and were subsequently discharged from the hospital. Of note, close observations of individual patients during the hospital stay and whole bowel irrigation were the most effective intervention in nearly all of the cases.
Discussion
This study was conducted to investigate the clinical presentations, diagnoses, management and therapeutic measures, and the clinical outcomes in 86 body packers and body stuffers during the admission and hospital stay. In both groups, the patients were primarily young men with a prior history of substance abuse and dependency. Heroin was the most commonly concealed drug, and none of the cases underwent surgery or endoscopy to remove the drug packets, and all of them were discharged from the hospital in full recovery. In other studies, the most common type of substances has also been heroin [
8,
9]. In another study, the most smuggled substance was cocaine, followed by heroin, methamphetamines and cannabinoids [
3].
Smuggling illegal substances by internal concealment presents a global challenge for social and security institutions [
4,
5]. Improvements in packaging methods have significantly reduced the risk of rupture and possibility of detection [
6]. Most body packers do not voluntarily visit hospitals because of the successful concealment through advanced packaging systems. Such packages are easily excreted either through normal defecation at a desired destination, or due to fear of legal and judicial consequences [
7].
Our hospital, having well-equipped and specialized poisoning department, emergency room, wards, and intensive care units, has been a major referral center for many suspected body packers by the police, prisons and airports. The sample size used in this study is one of its strengths compared to those in other studies [
10-
12]. In this study, the most common contents of the packages were heroin and crystal methamphetamines, as identified by the hospital’s expert personnel. This is in contrast with previous Iranian studies, in which opium had been the most common concealed substance [
13,
14]. Further, almost all studies conducted in other countries have reported cocaine as being the most commonly smuggled drug by body packers [
10]. A primary reason that there was zero fatal outcome among these patients could be due to the content of the packages. In other international studies, fatal outcomes have been mainly from ruptured cocaine-containing packages, since poisoning with this substance is severe and often leads to death of the victims. Other reasons for death could be due to the numbers and quantity of concealed packages. Fortunately, in our study, the zero fatality was likely due to fewer packets and smaller amounts of concealed drugs compared to those reported in other studies [
7].
The efficacy of abdominal X-ray imaging to detect concealed packages in body packers and stuffers remains controversial. Previous studies have reported a broad spectrum of sensitivity for this method, ranging from 40 to 100% [
1,
9,
15]. Regardless of the sensitivity, many reports suggest that abdominal X-ray imaging has low efficiency to detect such packets in the body [
1,
2,
15]. In this study, abdominal X-ray was effective in detecting the packets in only 10 patients (14.7%) of the body stuffers and 11 cases (61.1%) of the body packers. The cumulative sensitivity of this method in both groups was 24.4% (n=21). It appears that the ability of X-ray imaging in detecting packets largely depends on the size, number, content and sealed materials. Conversely, CT scanning was able to detect concealed packages in the body and correctly identify the numbers in a total of 26 out of 86 individuals. This suggest that CT scanning was slightly more sensitive in detecting body packets than that of the X-ray method in this study.
In the current study, all cases of concealed packages by oral route were little in size and few in numbers. This was primarily to avoid detection by the police during the arrests or while leaving the prison. Another reason that small numbers of body packers and stuffers were referred to our hospital was that Isfahan is not a border city. The reasons cited here may justify the fact that few diagnostic methods and invasive therapeutic measures were employed in this study. Further, improvements in the quality of packaging for drugs in Western countries and surgical complications are among the reasons for conservative management approaches being popular in these cases [
10,
11]. The false negative rates in asymptomatic patients undergoing such treatments have been estimated at approximately 5%. Also, endoscopic intervention is not often suggested, because it has a high risk of package rupture [
15,
16]. This method was not used for any of the patients whose records were investigated in this study.
Conclusions
No patient in this study required endoscopy or surgery and there were no fatal outcomes. Computed tomography scanning was found to be more sensitive than abdominal X-ray imaging in detecting the smuggled packets. Close observation of the victims and whole bowel irrigation appeared to be adequate approaches for almost all cases, which resulted in full patient recovery and discharge from the hospital.
We assessed patients’ documents retrospectively, which could be considered as a limitation of the study. Also, it was not possible for us to confirm the diagnoses for body packers or stuffer’s directly from the involved physicians. In this study, we made the confirmation by checking the patients’ records or the police reports.
Ethical Considerations
Compliance with ethical guidelines
The authors observed all of the institutional guidelines on ethical aspects of using medical records, reflecting no untoward reports by the victims or the hospital staff on the investigated cases.The Ethics Committee at Isfahan University of Medical Sciences approved the study protocol.
Funding
The present manuscript was extracted from the MD. dissertation of the third author at the Department of Clinical Toxicology, School of Medicine, Isfahan University of Medical Sciences, Isfahan (Research project ID: 297069).
Author's contributions
Conceptualization and supervision: Farzad Gheshlaghi; Methodology: Mojgan Gomari; Data collection: Mojgan Gomari and Shayan Gheshlaghi: Data analysis: Farzad Gheshlaghi and Mijgan Gomari; Investigation, writing – original draft, and writing – review & editing, funding acquisition and resources: All authors
Conflict of interest
The authors declared no conflict of interests.
Acknowledgements
The authors would like to thank the staffs of Clinical Toxicology Department, Isfahan Clinical Toxicology Research Center and colleagues of the Archive Center at Khorshid hospital for their cooperation.
References










































 , Mojgan Gomari2
, Mojgan Gomari2 

 , Shaun L. Greene3
, Shaun L. Greene3 

 , Joe Anthony Rotella4
, Joe Anthony Rotella4 

 , Shayan Gheshlaghi *5
, Shayan Gheshlaghi *5 




-_5_year.PNG)