1. Guengerich FP. Mechanisms of drug toxicity and relevance to pharmaceutical development. Drug metabolism and pharmacokinetics. 2011;26(1):3-14. [
DOI:10.2133/dmpk.DMPK-10-RV-062] [
PMID] [
PMCID]
2. Borzelleca JF. Paracelsus: herald of modern toxicology. Toxicological sciences : an official journal of the Society of Toxicology. 2000;53(1):2-4. [
DOI:10.1093/toxsci/53.1.2] [
PMID]
3. Lian Y, Zhao J, Wang YM, Zhao J, Peng SQ. Metallothionein protects against isoniazid-induced liver injury through the inhibition of CYP2E1-dependent oxidative and nitrosative impairment in mice. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2017;102:32-8. [
DOI:10.1016/j.fct.2017.01.016] [
PMID]
4. Hassan HM, Guo H, Yousef BA, Ping-Ping D, Zhang L, Jiang Z. Dexamethasone Pretreatment Alleviates Isoniazid/Lipopolysaccharide Hepatotoxicity: Inhibition of Inflammatory and Oxidative Stress. Frontiers in pharmacology. 2017;8:133. [
DOI:10.3389/fphar.2017.00133] [
PMID] [
PMCID]
5. Wang Z, Yao T, Pini M, Zhou Z, Fantuzzi G, Song Z. Betaine improved adipose tissue function in mice fed a high-fat diet: a mechanism for hepatoprotective effect of betaine in nonalcoholic fatty liver disease. American journal of physiology Gastrointestinal and liver physiology. 2010;298(5):G634-42. [
DOI:10.1152/ajpgi.00249.2009] [
PMID] [
PMCID]
6. Khodayar MJ, Kalantari H, Khorsandi L, Rashno M, Zeidooni L. Betaine protects mice against acetaminophen hepatotoxicity possibly via mitochondrial complex II and glutathione availability. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2018;103:1436-45. [
DOI:10.1016/j.biopha.2018.04.154] [
PMID]
7. Heidari R, Niknahad H, Sadeghi A, Mohammadi H, Ghanbarinejad V, Ommati MM, et al. Betaine treatment protects liver through regulating mitochondrial function and counteracting oxidative stress in acute and chronic animal models of hepatic injury. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2018;103:75-86. [
DOI:10.1016/j.biopha.2018.04.010] [
PMID]
8. Hasanzadeh Moghadam M, Khadem Ansari MH, Farjah GH, Rasmi Y. Hepatoprotective effects of betaine on liver damages followed by myocardial infarction. Vet Res Forum. 2018;9(2):129-35.
9. Jung YS, Kim SJ, Kwon DY, Ahn CW, Kim YS, Choi DW, et al. Alleviation of alcoholic liver injury by betaine involves an enhancement of antioxidant defense via regulation of sulfur amino acid metabolism. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2013;62:292-8. [
DOI:10.1016/j.fct.2013.08.049] [
PMID]
10. Ghartavol MM, Gholizadeh-Ghaleh Aziz S, Babaei G, Hossein Farjah G, Hassan Khadem Ansari M. The protective impact of betaine on the tissue structure and renal function in isoproterenol-induced myocardial infarction in rat. Molecular genetics & genomic medicine. 2019;7(4):e00579. [
DOI:10.1002/mgg3.579] [
PMID] [
PMCID]
11. Eminzade S, Uraz F, Izzettin FV. Silymarin protects liver against toxic effects of anti-tuberculosis drugs in experimental animals. Nutrition & metabolism. 2008;5:18. [
DOI:10.1186/1743-7075-5-18] [
PMID] [
PMCID]
12. Basheer AS, Siddiqui A, Paudel YN, Hassan MQ, Imran M, Najmi AK. Hepatoprotective and antioxidant effects of fish oil on isoniazid-rifampin induced hepatotoxicity in rats. Pharma Nutrit. 2017;5:29-33. [
DOI:10.1016/j.phanu.2017.01.002]
13. Sedlak J, Lindsay RH. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman's reagent. Analytical biochemistry. 1968;25(1):192-205. [
DOI:10.1016/0003-2697(68)90092-4] [
PMID]
14. Beutler E, Duron O, Kelly Bm. An improved method for the determination of blood glutathione. J Lab Clin Med. 1963;61:882-8.
15. Chance B, Oshino N. Kinetics and mechanisms of catalase in peroxisomes of the mitochondrial fraction. The Biochemical journal. 1971;122(2):225-33. [
DOI:10.1042/bj1220225] [
PMID] [
PMCID]
16. Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Analytical biochemistry. 1979;95(2):351-8. [
DOI:10.1016/0003-2697(79)90738-3] [
PMID]
17. Misra HP, Fridovich I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. The Journal of biological chemistry. 1972;247(10):3170-5. [
DOI:10.1016/S0021-9258(19)45228-9]
18. Metushi I, Uetrecht J, Phillips E. Mechanism of isoniazid-induced hepatotoxicity: then and now. British journal of clinical pharmacology. 2016;81(6):1030-6. [
DOI:10.1111/bcp.12885] [
PMID] [
PMCID]
19. Hassan HM, Guo H, Yousef B, Guerram M, Hamdi AM, Zhang L. Role of Inflammatory and Oxidative Stress, Cytochrome P450 2E1, and Bile Acid Disturbance in Rat Liver Injury Induced by Isoniazid and Lipopolysaccharide Cotreatment. Antimicrob Agent Chemother. 2016;60(9):5285-93. [
DOI:10.1128/AAC.00854-16] [
PMID] [
PMCID]
20. Metushi IG, Sanders C, Acute Liver Study G, Lee WM, Uetrecht J. Detection of anti-isoniazid and anti-cytochrome P450 antibodies in patients with isoniazid-induced liver failure. Hepatology. 2014;59(3):1084-93. [
DOI:10.1002/hep.26564] [
PMID] [
PMCID]
21. Metushi IG, Cai P, Zhu X, Nakagawa T, Uetrecht JP. A fresh look at the mechanism of isoniazid-induced hepatotoxicity. Clinical pharmacology and therapeutics. 2011;89(6):911-4. [
DOI:10.1038/clpt.2010.355] [
PMID]
22. Okwa IB, Akindele AJ, Agbaje EO, Oshinuga OT, Anunobi CC, Adeyemi OO. Effect of subclinical, clinical, and supraclinical doses of calcium channel blockers on models of drug-induced hepatotoxicity in rats. EXCLI J. 2013;12:231-50.
23. Sallie R, Tredger JM, Williams R. Drugs and the liver. Part 1: Testing liver function. Biopharmaceutics & drug disposition. 1991;12(4):251-9. [
DOI:10.1002/bdd.2510120403] [
PMID]
24. Hassan HM, Guo HL, Yousef BA, Luyong Z, Zhenzhou J. Hepatotoxicity mechanisms of isoniazid: A mini-review. Journal of applied toxicology : JAT. 2015;35(12):1427-32. [
DOI:10.1002/jat.3175] [
PMID]
25. Evan Prince S, Udhaya LB, Sunitha PS, Arumugam G. Reparation of Isoniazid and Rifampicin Combinatorial Therapy-Induced Hepatotoxic Effects by Bacopa monnieri. Pharmacology. 2016;98(1-2):29-34. [
DOI:10.1159/000444856] [
PMID]
26. Kim SK, Kim YC, Kim YC. Effects of singly administered betaine on hepatotoxicity of chloroform in mice. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 1998;36(8):655-61. [
DOI:10.1016/S0278-6915(98)00024-6] [
PMID]
27. Balkan J, Parldar FH, Dogru-Abbasoglu S, Aykac-Toker G, Uysal M. The effect of taurine or betaine pretreatment on hepatotoxicity and prooxidant status induced by lipopolysaccharide treatment in the liver of rats. European journal of gastroenterology & hepatology. 2005;17(9):917-21. [
DOI:10.1097/00042737-200509000-00006] [
PMID]
28. Sodhi CP, Rana SV, Mehta SK, Vaiphei K, Attari S, Mehta S. Study of oxidative-stress in isoniazid-rifampicin induced hepatic injury in young rats. Drug and chemical toxicology. 1997;20(3):255-69. [
DOI:10.3109/01480549709003881] [
PMID]
29. Palanisamy N, Manian S. Protective effects of Asparagus racemosus on oxidative damage in isoniazid-induced hepatotoxic rats: an in vivo study. Toxicology and industrial health. 2012;28(3):238-44. [
DOI:10.1177/0748233711410911] [
PMID]
30. Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI. The central role of glutathione in the pathophysiology of human diseases. Archives of physiology and biochemistry. 2007;113(4-5):234-58. [
DOI:10.1080/13813450701661198] [
PMID]
31. Ramappa V, Aithal GP. Hepatotoxicity Related to Anti-tuberculosis Drugs: Mechanisms and Management. Journal of clinical and experimental hepatology. 2013;3(1):37-49. [
DOI:10.1016/j.jceh.2012.12.001] [
PMID] [
PMCID]
32. Viswanatha Swamy AH, Kulkarni RV, Thippeswamy AH, Koti BC, Gore A. Evaluation of hepatoprotective activity of Cissus quadrangularis stem extract against isoniazid-induced liver damage in rats. Indian journal of pharmacology. 2010;42(6):397-400. [
DOI:10.4103/0253-7613.71920] [
PMID] [
PMCID]
33. Ishida Y, Kondo T, Ohshima T, Fujiwara H, Iwakura Y, Mukaida N. A pivotal involvement of IFN-gamma in the pathogenesis of acetaminophen-induced acute liver injury. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2002;16(10):1227-36. [
DOI:10.1096/fj.02-0046com] [
PMID]
34. Tarantino G, Savastano S, Colao A. Hepatic steatosis, low-grade chronic inflammation and hormone/growth factor/adipokine imbalance. World journal of gastroenterology. 2010;16(38):4773-83. [
DOI:10.3748/wjg.v16.i38.4773] [
PMID] [
PMCID]
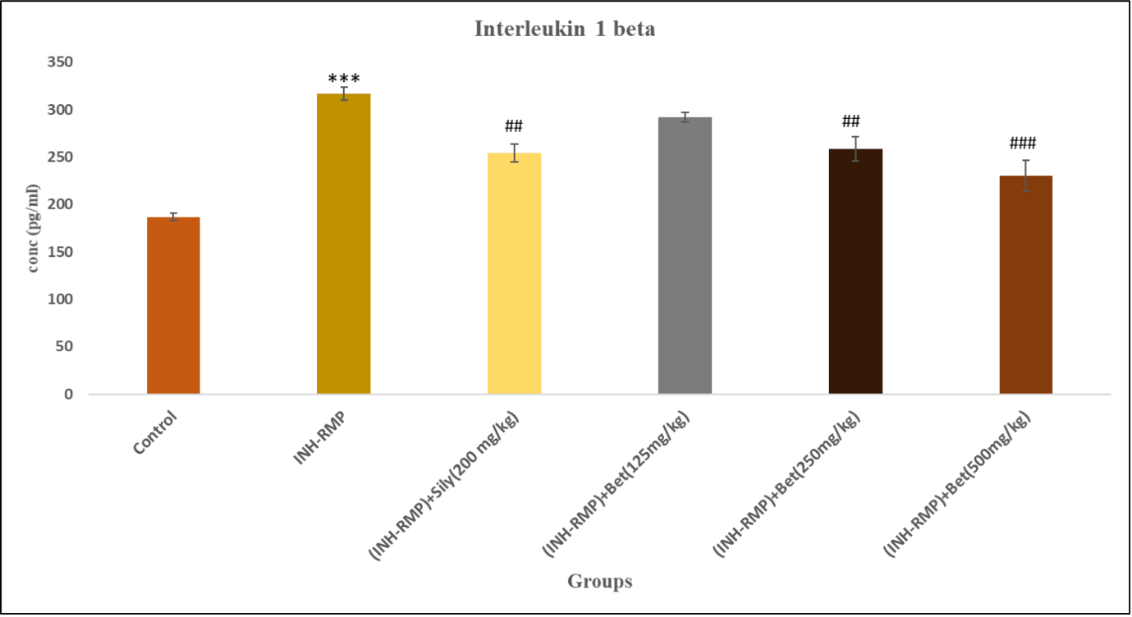
35. Dinarello CA. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117(14):3720-32. [
DOI:10.1182/blood-2010-07-273417] [
PMID] [
PMCID]
36. Dinarello CA. An expanding role for interleukin-1 blockade from gout to cancer. Molecular medicine. 2014;20 Suppl 1(Suppl 1):S43-58. [
DOI:10.2119/molmed.2014.00232] [
PMID] [
PMCID]
37. Tacke F, Luedde T, Trautwein C. Inflammatory pathways in liver homeostasis and liver injury. Clinical reviews in allergy & immunology. 2009;36(1):4-12. [
DOI:10.1007/s12016-008-8091-0] [
PMID]