1. Alabi OA, Ologbonjaye KI, Awosolu O, Alalade OE. Public and Environmental Health Effects of Plastic Wastes Disposal: A Review. J Toxicol Risk Assess. 2019;5:021. [
DOI:10.23937/2572-4061.1510021]
2. Yuan Z, Nag R, Cummins E. Human health concerns regarding microplastics in the aquatic environment - From marine to food systems. The Science of the total environment. 2022;823:153730. [
DOI:10.1016/j.scitotenv.2022.153730] [
PMID]
3. Baralic K, Buha Djordjevic A, Zivancevic K, Antonijevic E, Andelkovic M, Javorac D, et al. Toxic Effects of the Mixture of Phthalates and Bisphenol A-Subacute Oral Toxicity Study in Wistar Rats. International journal of environmental research and public health. 2020;17(3). [
DOI:10.3390/ijerph17030746] [
PMID] [
PMCID]
4. Giuliani A, Zuccarini M, Cichelli A, Khan H, Reale M. Critical Review on the Presence of Phthalates in Food and Evidence of Their Biological Impact. Intl J Environ Res Pub Health. 2020;17(16):5655. [
DOI:10.3390/ijerph17165655] [
PMID] [
PMCID]
5. Hahladakis JN, Velis CA, Weber R, Iacovidou E, Purnell P. An overview of chemical additives present in plastics: Migration, release, fate and environmental impact during their use, disposal and recycling. Journal of hazardous materials. 2018;344:179-99. [
DOI:10.1016/j.jhazmat.2017.10.014] [
PMID]
6. Muscogiuri G, Colao A. Phtalates: new cardiovascular health disruptors? Archives of toxicology. 2017;91(3):1513-7. [
DOI:10.1007/s00204-016-1780-1] [
PMID]
7. Lind PM, Zethelius B, Lind L. Circulating levels of phthalate metabolites are associated with prevalent diabetes in the elderly. Diabetes care. 2012;35(7):1519-24. [
DOI:10.2337/dc11-2396] [
PMID] [
PMCID]
8. Fiore M, Oliveri CG, Caltabiano R, Buffone A, Zuccarello P, Cormaci L. Role of Emerging Environmental Risk Factors in Thyroid Cancer: A Brief Review. Intl J Environ Res Pub Health. 2019;16:1185. [
DOI:10.3390/ijerph16071185] [
PMID] [
PMCID]
9. Miao Y, Wang R, Lu C, Zhao J, Deng Q. Lifetime cancer risk assessment for inhalation exposure to di(2-ethylhexyl) phthalate (DEHP). Environmental science and pollution research international. 2017;24(1):312-20. [
DOI:10.1007/s11356-016-7797-4] [
PMID]
10. Zhu M, Huang C, Ma X, Wu R, Zhu W, Li X, et al. Phthalates promote prostate cancer cell proliferation through activation of ERK5 and p38. Environmental toxicology and pharmacology. 2018;63:29-33. [
DOI:10.1016/j.etap.2018.08.007] [
PMID]
11. Kautzky-Willer A, Harreiter J, Pacini G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocrine reviews. 2016;37(3):278-316. [
DOI:10.1210/er.2015-1137] [
PMID] [
PMCID]
12. Jaimes R, Swiercz A, Sherman M, Muselimyan N, Marvar PJ, Posnack NG. Plastics and cardiovascular health: Phthalates may disrupt heart rate variability and cardiovascular reactivity. Am J Physiol Heart Circ Physiol. 2017;313:1044-53. [
DOI:10.1152/ajpheart.00364.2017] [
PMID] [
PMCID]
13. Shih MF, Pan KH, Cherng JY. Possible mechanisms of di(2-ethylhexyl) phthalate-induced mmp-2 and mmp-9 expression in a 7r5 rat vascular smooth muscle cells. Intl J Mol Sci. 2015;16:28800-11. [
DOI:10.3390/ijms161226131] [
PMID] [
PMCID]
14. Wood CE, Jokinen MP, Johnson CL, Olson GR, Hester S, George M, et al. Comparative time course profiles of phthalate stereoisomers in mice. Toxicological sciences : an official journal of the Society of Toxicology. 2014;139(1):21-34. [
DOI:10.1093/toxsci/kfu025] [
PMID]
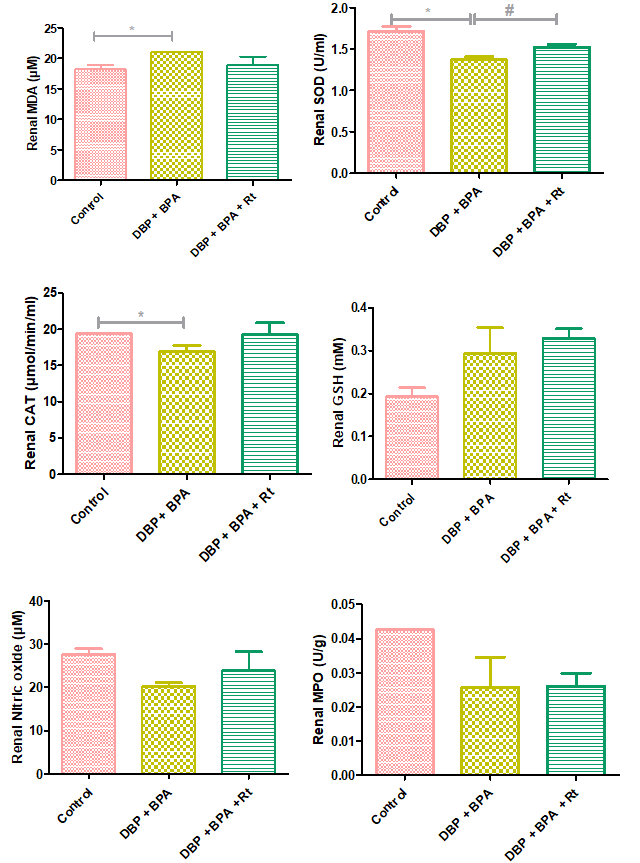
15. Wu CT, Wang CC, Huang LC, Liu SH, Chiang CK. Plasticizer Di-(2-Ethylhexyl)Phthalate Induces Epithelial-to-Mesenchymal Transition and Renal Fibrosis In Vitro and In Vivo. Toxicological sciences : an official journal of the Society of Toxicology. 2018;164(1):363-74. [
DOI:10.1093/toxsci/kfy094] [
PMID]
16. Posnack NG. The adverse cardiac effects of Di(2-ethylhexyl)phthalate and Bisphenol A. Cardiovascular toxicology. 2014;14(4):339-57. [
DOI:10.1007/s12012-014-9258-y] [
PMID] [
PMCID]
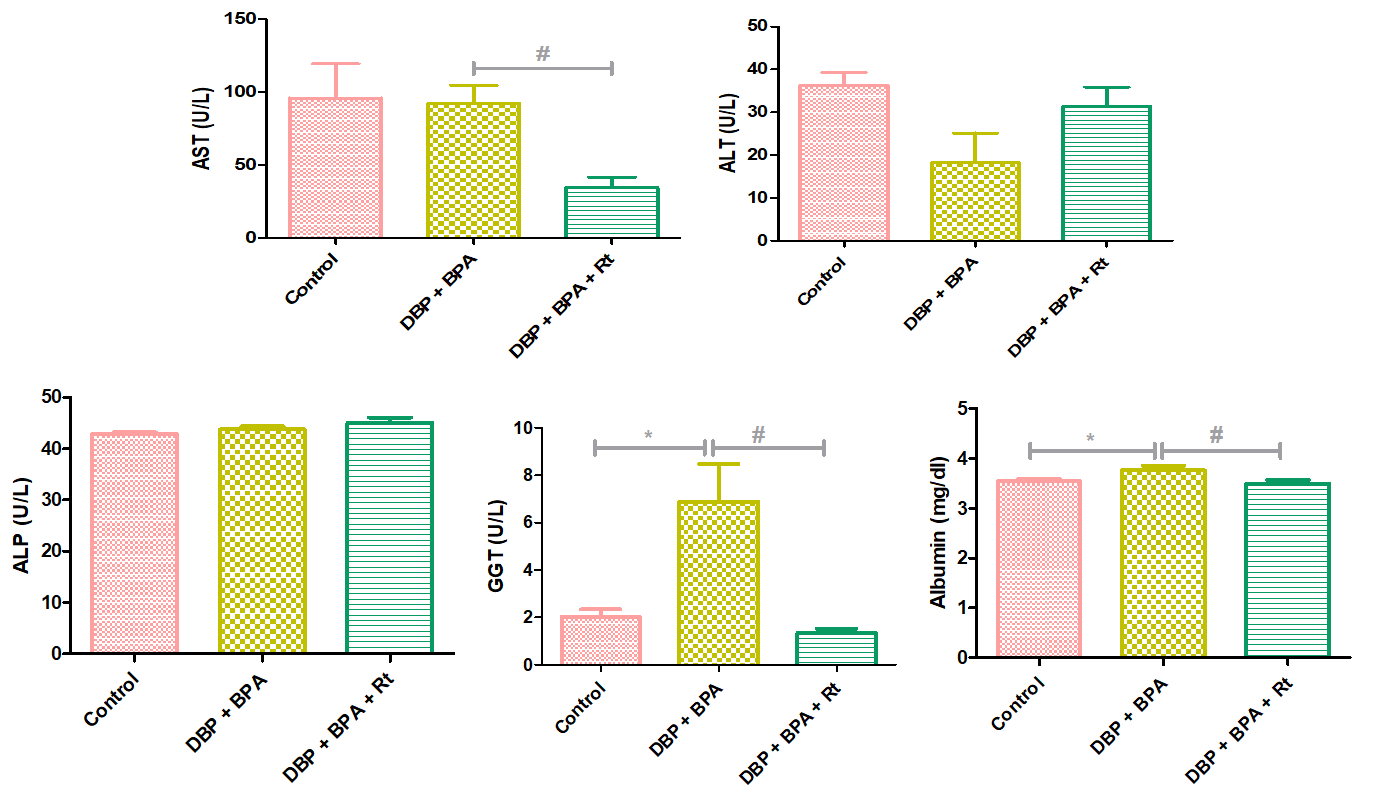
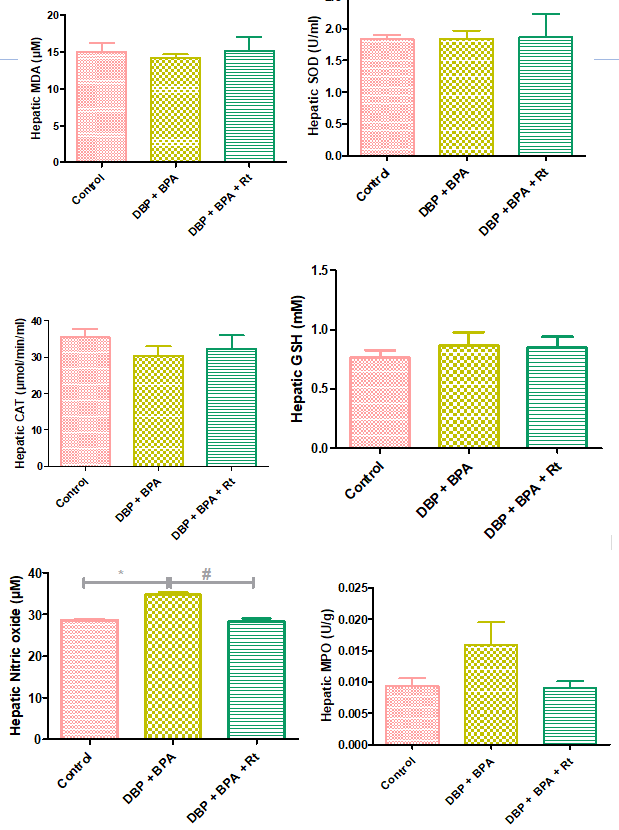
17. Oluranti OI, Alabi BA, Michael OS, Ojo AO, Fatokun BP. Rutin prevents cardiac oxidative stress and inflammation induced by bisphenol A and dibutyl phthalate exposure via NRF-2/NF-kappaB pathway. Life sciences. 2021;284:119878. [
DOI:10.1016/j.lfs.2021.119878] [
PMID]
18. Xia Y, Zweier JL. Measurement of myeloperoxidase in leukocyte-containing tissues. Analytical biochemistry. 1997;245(1):93-6. [
DOI:10.1006/abio.1996.9940] [
PMID]
19. Knez J. Endocrine-disrupting chemicals and male reproductive health. Reprod BioMed. 2013;26:440-8. [
DOI:10.1016/j.rbmo.2013.02.005] [
PMID]
20. Moustafa GG, Ahmed AAM. Impact of prenatal and postnatal exposure to bisphenol A on female rats in a two generational study: Genotoxic and immunohistochemical implications. Toxicology reports. 2016;3:685-95. [
DOI:10.1016/j.toxrep.2016.08.008] [
PMID] [
PMCID]
21. Abdel-Rahman HG, Abdelrazek HMA, Zeidan DW, Mohamed RM, Abdelazim AM. Lycopene: Hepatoprotective and Antioxidant Effects toward Bisphenol A-Induced Toxicity in Female Wistar Rats. Oxidative medicine and cellular longevity. 2018;2018:5167524. [
DOI:10.1155/2018/5167524] [
PMID] [
PMCID]
22. Baralic K, Zivancevic K, Javorac D, Buha Djordjevic A, Andelkovic M, Jorgovanovic D, et al. Multi-strain probiotic ameliorated toxic effects of phthalates and bisphenol A mixture in Wistar rats. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2020;143:111540. [
DOI:10.1016/j.fct.2020.111540] [
PMID]
23. Khan RA, Khan MR, Sahreen S. CCl4-induced hepatotoxicity: protective effect of rutin on p53, CYP2E1 and the antioxidative status in rat. BMC complementary and alternative medicine. 2012;12:178. [
DOI:10.1186/1472-6882-12-178] [
PMID] [
PMCID]
24. Reddy MK, Reddy AG, Kumar BK, Madhuri D, Boobalan G, Reddy MA. Protective effect of rutin in comparison to silymarin against induced hepatotoxicity in rats. Veterinar World. 2017;10(1):74-80. [
DOI:10.14202/vetworld.2017.74-80] [
PMID] [
PMCID]
25. Gelen V, Şengül E, Gedikli S, Atila G, Uslu H, Makav M. The protective effect of rutin and quercetin on 5-FU-induced hepatotoxicity in rats. Asia Pacific J Tropic Biomed. 2017;7(7):647-53. [
DOI:10.1016/j.apjtb.2017.06.013]
26. Tanko Y, Jimoh A, Sulaiman I, Mohammed KA, Salisu AI, Yusuf R. The Effect of Rutin on Lipid Profile and Liver Function Enzymes on Alloxan Induced Hyperglycaemic Wistar Rats Bajopas. 2017;10(1):210-4. [
DOI:10.4314/bajopas.v10i1.30]
27. Ahmed OM, Galaly SR, Mostafa MMA, Eed EM, Ali TM, Fahmy AM, et al. Thyme Oil and Thymol Counter Doxorubicin-Induced Hepatotoxicity via Modulation of Inflammation, Apoptosis, and Oxidative Stress. Oxidative medicine and cellular longevity. 2022;2022:6702773.
https://doi.org/10.1155/2022/6702773 [
DOI:10.1155/2022/2710607] [
PMID] [
PMCID]
28. Elsawy H, Badr GM, Sedky A, Abdallah BM, Alzahrani AM, Abdel-Moneim AM. Rutin ameliorates carbon tetrachloride (CCl(4))-induced hepatorenal toxicity and hypogonadism in male rats. PeerJ. 2019;7:e7011. [
DOI:10.7717/peerj.7011] [
PMID] [
PMCID]
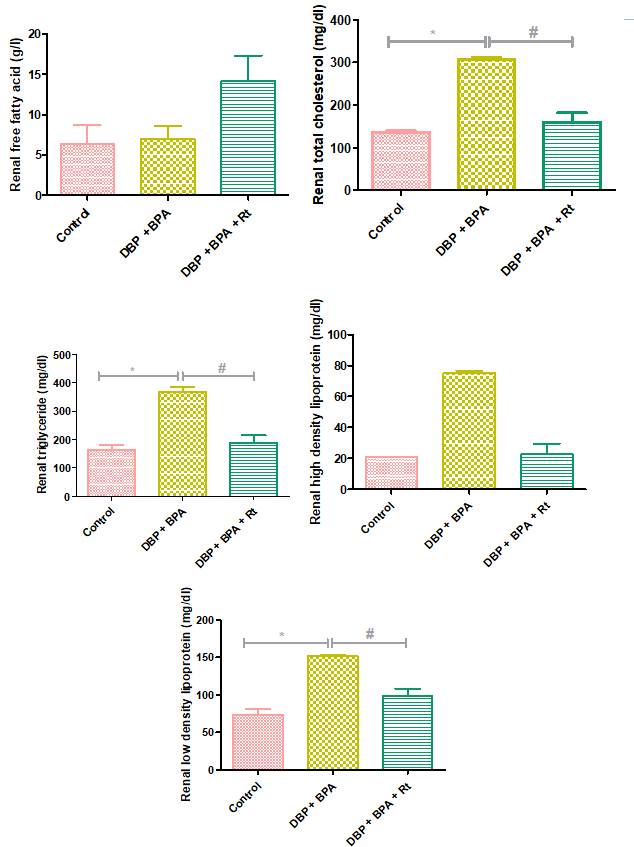
29. Alhoshani AR, Hafez MM, Husain S, Al-Sheikh AM, Alotaibi MR, Al Rejaie SS, et al. Protective effect of rutin supplementation against cisplatin-induced Nephrotoxicity in rats. BMC nephrology. 2017;18(1):194. [
DOI:10.1186/s12882-017-0601-y] [
PMID] [
PMCID]
30. Khajevand-Khazaei MR, Mohseni-Moghaddam P, Hosseini M, Gholami L, Baluchnejadmojarad T, Roghani M. Rutin, a quercetin glycoside, alleviates acute endotoxemic kidney injury in C57BL/6 mice via suppression of inflammation and up-regulation of antioxidants and SIRT1. European journal of pharmacology. 2018;833:307-13. [
DOI:10.1016/j.ejphar.2018.06.019] [
PMID]
31. Hassan ZK, Elobeid MA, Virk P, Omer SA, ElAmin M, Daghestani MH, et al. Bisphenol A induces hepatotoxicity through oxidative stress in rat model. Oxidative medicine and cellular longevity. 2012;2012:194829. [
DOI:10.1155/2012/194829] [
PMID] [
PMCID]
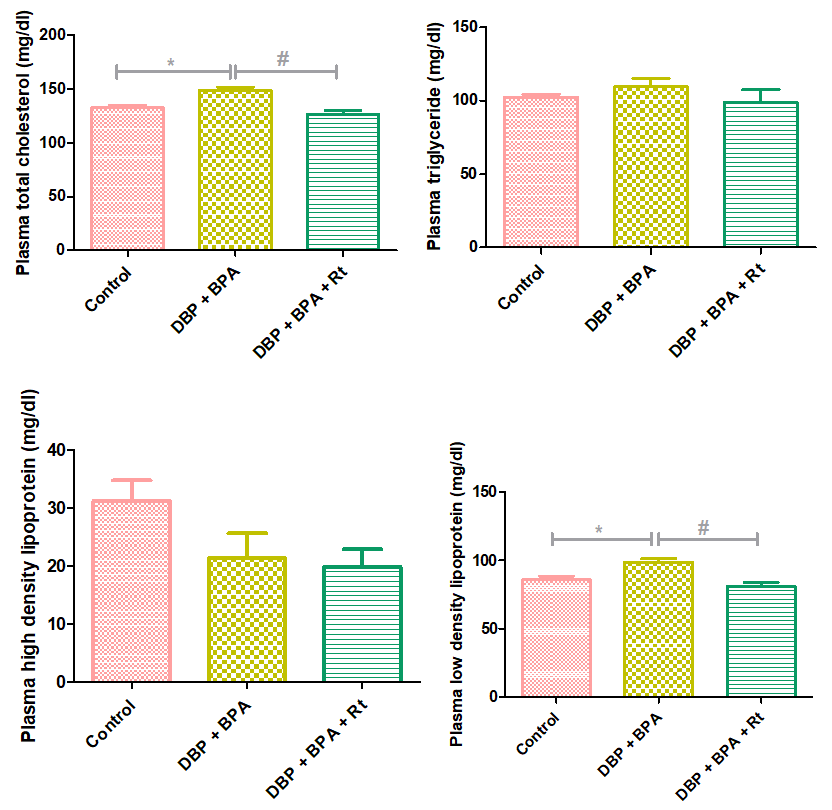
32. Moghaddam HS, Samarghandian S, Farkhondeh T. Effect of bisphenol A on blood glucose, lipid profile and oxidative stress indices in adult male mice. Toxicology mechanisms and methods. 2015;25(7):507-13. [
DOI:10.3109/15376516.2015.1056395] [
PMID]
33. Vanani AR, Mahdavinia M, Shirani M, Alizadeh S, Dehghani MA. Protective effects of quercetin against oxidative stress induced by bisphenol-A in rat cardiac mitochondria. Environmental science and pollution research international. 2020;27(13):15093-102. [
DOI:10.1007/s11356-020-08048-0] [
PMID]
34. Celik H, Kandemir FM, Caglayan C, Ozdemir S, Comakli S, Kucukler S, et al. Neuroprotective effect of rutin against colistin-induced oxidative stress, inflammation and apoptosis in rat brain associated with the CREB/BDNF expressions. Molecular biology reports. 2020;47(3):2023-34. [
DOI:10.1007/s11033-020-05302-z] [
PMID]
35. Singh S, Dubey V, Meena A, Siddiqui L, Maurya AK, Luqman S. Rutin restricts hydrogen peroxide-induced alterations by up-regulating the redox-system: An in vitro, in vivo and in silico study. European journal of pharmacology. 2018;835:115-25. [
DOI:10.1016/j.ejphar.2018.07.055] [
PMID]
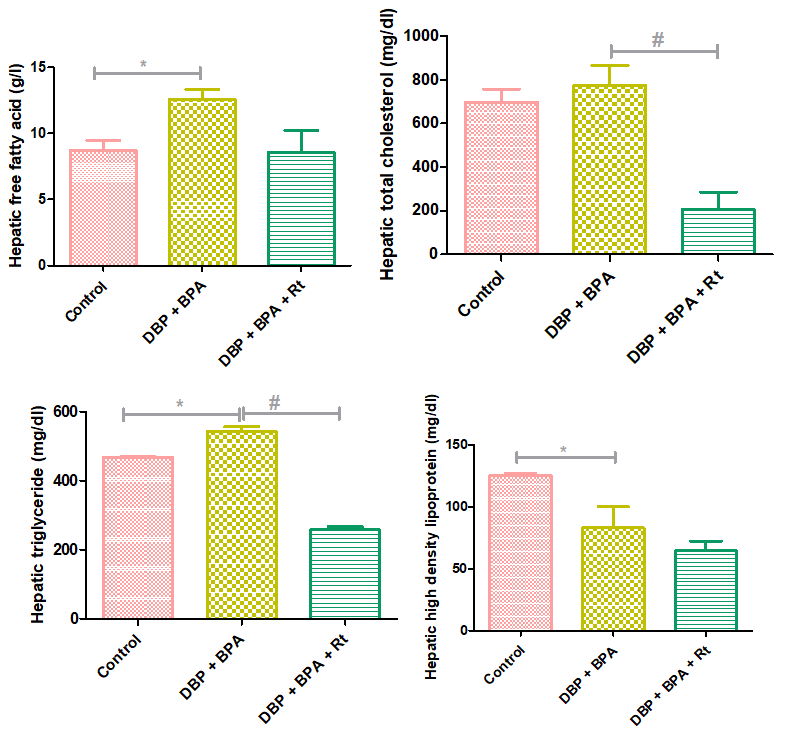
36. Lin Y, Ding D, Huang Q, Liu Q, Lu H, Lu Y, et al. Downregulation of miR-192 causes hepatic steatosis and lipid accumulation by inducing SREBF1: Novel mechanism for bisphenol A-triggered non-alcoholic fatty liver disease. Biochimica et biophysica acta Molecular and cell biology of lipids. 2017;1862(9):869-82. [
DOI:10.1016/j.bbalip.2017.05.001] [
PMID]
37. Hassani FV, Mehri S, Abnous K, Birner-Gruenberger R, Hosseinzadeh H. Protective effect of crocin on BPA-induced liver toxicity in rats through inhibition of oxidative stress and down-regulation of MAPK and MAPKAP signaling pathway and miRNA-122 expression. Food Chem Toxicol. 2017;107:395-405. [
DOI:10.1016/j.fct.2017.07.007] [
PMID]
38. Eweda SM, Newairy ASA, Abdou HM, Gaber AS. Bisphenol A-induced oxidative damage in the hepatic and cardiac tissues of rats: The modulatory role of sesame lignans. Experimental and therapeutic medicine. 2020;19(1):33-44. [
DOI:10.3892/etm.2019.8193] [
PMID] [
PMCID]
39. Fadishei M, Ghasemzadeh Rahbardar M, Imenshahidi M, Mohajeri A, Razavi BM, Hosseinzadeh H. Effects of Nigella sativa oil and thymoquinone against bisphenol A-induced metabolic disorder in rats. Phytotherapy research : PTR. 2021;35(4):2005-24. [
DOI:10.1002/ptr.6944] [
PMID]
40. Marmugi A, Ducheix S, Lasserre F, Polizzi A, Paris A, Priymenko N, et al. Low doses of bisphenol A induce gene expression related to lipid synthesis and trigger triglyceride accumulation in adult mouse liver. Hepatology. 2012;55(2):395-407. [
DOI:10.1002/hep.24685] [
PMID]
41. Hsu CL, Wu CH, Huang SL, Yen GC. Phenolic compounds rutin and o-coumaric acid ameliorate obesity induced by high-fat diet in rats. J Agricultur Food Chemist. 2009;57(2):425-31. [
DOI:10.1021/jf802715t] [
PMID]
42. Wu CH, Lin MC, Wang HC, Yang MY, Jou MJ, Wang CJ. Rutin inhibits oleic acid induced lipid accumulation via reducing lipogenesis and oxidative stress in hepatocarcinoma cells. Journal of food science. 2011;76(2):T65-72. [
DOI:10.1111/j.1750-3841.2010.02033.x]
43. Liu Q, Pan R, Ding L, Zhang F, Hu L, Ding B, et al. Rutin exhibits hepatoprotective effects in a mouse model of non-alcoholic fatty liver disease by reducing hepatic lipid levels and mitigating lipid-induced oxidative injuries. International immunopharmacology. 2017;49:132-41. [
DOI:10.1016/j.intimp.2017.05.026] [
PMID]
44. Raja NR, Nair AR, Senthilpandian S, Ravi V. Hypolipidemic action of Rutin on Triton WR-1339-induced hyperlipidemia in rats. J Pre-clin & Clin Res. 2021;15(2):51-5. [
DOI:10.26444/jpccr/136231]
45. Jung CH, Cho I, Ahn J, Jeon TI, Ha TY. Quercetin reduces high-fat diet-induced fat accumulation in the liver by regulating lipid metabolism genes. Phytotherapy research : PTR. 2013;27(1):139-43. [
DOI:10.1002/ptr.4687] [
PMID]










































 , Praise Akin-Aborishade2
, Praise Akin-Aborishade2 

 , Atilola Olarinde2
, Atilola Olarinde2 

 , Babatunde Alabi3
, Babatunde Alabi3 

 , Esther Ojo-Ayangoke2
, Esther Ojo-Ayangoke2 

 , Timilehin Mayowa2
, Timilehin Mayowa2 

 , Marvelous Paseda2
, Marvelous Paseda2 

 , Ayomide Lawal2
, Ayomide Lawal2 

 , Ibukun Dahunsi2
, Ibukun Dahunsi2